A client with schizophrenia is started on clozapine, embarking on a therapeutic journey that requires meticulous monitoring, patient education, and an understanding of potential adverse effects. This article delves into the complexities of clozapine therapy, empowering healthcare professionals with the knowledge to optimize treatment outcomes.
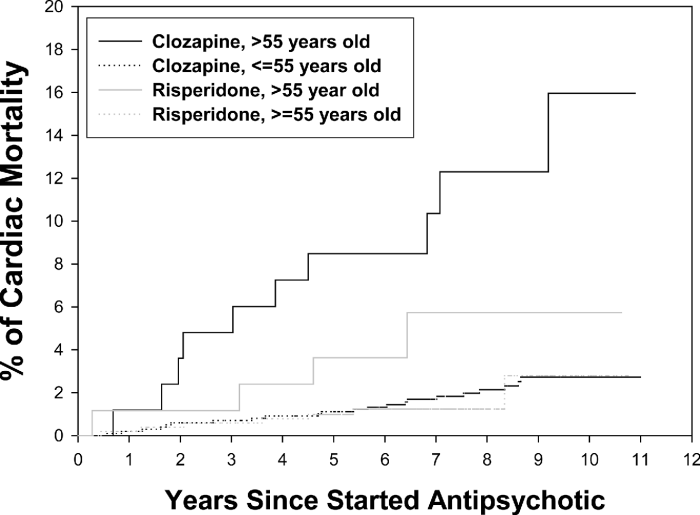
Clozapine, the “gold standard” for schizophrenia, offers unparalleled efficacy in reducing symptoms and preventing relapse. However, its use demands vigilance due to the risk of severe adverse effects, necessitating regular blood monitoring and careful management.
Clozapine: An Overview
Clozapine is an atypical antipsychotic medication belonging to the dibenzodiazepine class. It exerts its therapeutic effects by modulating dopamine and serotonin neurotransmission in the brain. Clozapine is primarily indicated for the treatment of schizophrenia, particularly in patients who have failed to respond to other antipsychotic medications.
Clozapine is often considered the “gold standard” treatment for schizophrenia due to its superior efficacy in reducing positive and negative symptoms, as well as its ability to improve cognitive function and social functioning.
Monitoring and Management of Clozapine Therapy: A Client With Schizophrenia Is Started On Clozapine
Importance of Regular Blood Monitoring, A client with schizophrenia is started on clozapine
Regular blood monitoring is crucial during clozapine treatment to detect potential adverse effects, particularly agranulocytosis, a rare but potentially life-threatening condition characterized by a severe reduction in white blood cell count.
The frequency of blood monitoring varies depending on the patient’s risk factors, but generally includes:
- Weekly monitoring for the first 18 weeks of treatment
- Biweekly monitoring for the next 6 months
- Monthly monitoring thereafter
Potential Adverse Effects
Clozapine is associated with several potential adverse effects, including:
- Agranulocytosis:A rare but serious condition that can lead to life-threatening infections
- Seizures:Clozapine has a higher risk of causing seizures compared to other antipsychotics
- Metabolic changes:Clozapine can increase the risk of weight gain, hyperglycemia, and hyperlipidemia
Management of Adverse Effects
Managing adverse effects of clozapine involves:
- Dose adjustments:Reducing the dose or discontinuing clozapine may be necessary in cases of severe adverse effects
- Discontinuation criteria:Treatment should be discontinued immediately if agranulocytosis or seizures occur
- Alternative treatment options:If clozapine is not tolerated, other antipsychotics or non-pharmacological interventions may be considered
Questions and Answers
What is the mechanism of action of clozapine?
Clozapine exerts its therapeutic effects by modulating neurotransmitter systems, particularly dopamine and serotonin, in the brain.
What are the potential adverse effects of clozapine?
Clozapine can cause severe adverse effects, including agranulocytosis, seizures, and metabolic changes, necessitating close monitoring.
How often should blood monitoring be performed during clozapine therapy?
Blood monitoring, including complete blood count and absolute neutrophil count, should be performed weekly for the first 6 months of treatment and monthly thereafter.